Functional Balance Training: Uneven and Unstable Surfaces
Whether you are a physical therapist, chiropractor, athletic trainer, Pilates instructor, or other type of fitness professional, it is likely that you work with clients and/or patients who need to improve their balance.
The evolution of balance training
Over the last three decades, balance training has evolved dramatically. Through the 90s and into the early 2000s, health and fitness professionals began to look more closely at the “functionality” of the exercises they were prescribing; that is, how exercises translate to movement outside of the clinic, studio or gym.
It was realized that balance training in a predictable, static environment would yield sub-par results. Because most individuals need to have sound balance while moving, people need to combine traditional static balance exercises with mobile, multiplanar and unpredictable dynamic exercises across variable surfaces.
This realization caused health and fitness professionals to do two things differently:
1.) They began incorporating more dynamic, functional movement into their programming.
2.) They began utilizing functional new forms of equipment to help their patients and clients achieve their goals.
Balance tools for functional training
Since the shift towards more functional forms of balance training, innovators have created an abundance of balance training tools. Most of these tools offer some sort of variable surface to conduct exercises on and/or across. The basic logic behind these products is simple: exercising on a variable surface will introduce unpredictable balance demands to the patient or client, helping them build a stronger neurological connection between the brain, feet, and everything in between.
Most balance training tools fall into one of two main categories: unstable surfaces and uneven surfaces.
Unstable surface balance tools
Unstable surfaces can be thought of as any surface that moves as the patient or client is standing on top of it. With this variability in movement, the body’s main sensory systems that govern balance (the vestibular and proprioceptive systems) are turned on to a greater degree. Over time, this enhanced sensory and muscle activation can build better balance, helping the individual develop a better intuitive understanding of their body’s position in space.
While a vast number of exercises can be conducted on top of a balance tool that offers an unstable surface, mobile exercises (such as walking or lunging) can be challenging since the surface area of these tools can be quite small.
Examples of balance tools that offer an unstable surface include wobble boards, balance pads, balance discs, and instability platforms. These tools each offer their own unique form of instability.
Wobble Boards
Wobble boards come in many shapes and sizes, but the concept is similar across all variations. The tools feature a solid surface on top of a curved base that moves in either one plane of motion (easier) or in all directions (harder). Wobble boards are great for all patient and client types. If you are in the market for a wobble board, the Wobblesmart by OPTP is a great option. It can be adjusted across 6 degrees of difficulty to accommodate a range of balance abilities, making it very versatile.
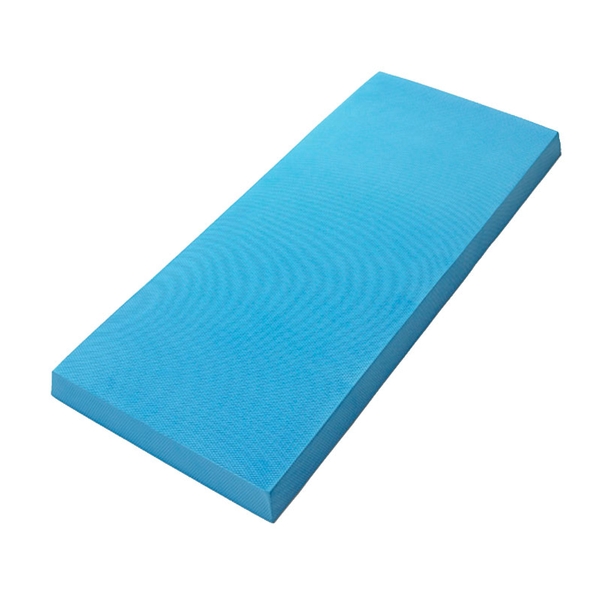
Balance Pads
Balance pads also come in many shapes and sizes. These balance tools are commonly made from pliable air-filled foam, which collapses as a user stands on top. Balance pads are most commonly used with older adults, since they offer a lesser degree of instability and are low to the ground, minimizing the risk of a fall. For a great balance pad option, check out the OPTP Pro Balance Pad.
Balance Discs
Balance discs are similar to both wobble boards and balance pads in that they can be made of collapsible foam or offer a solid platform on top of a curved base. They can also be completely air-filled. These tools are circular in shape and are commonly used in unilateral (single leg) exercises. For an exciting and unique balance disc option, check out the OPTP Dynamic Duo™ Balance & Stability Trainers.
Instability Platforms
Instability platforms include a broad range of dome-shaped balance tools. These products are most commonly made from a durable rubber material that is balloon-like, being filled with air. This rubber air filled “balloon” can serve as the balance tool itself or can be affixed to a solid platform that the user stands on top of. For one of the newest innovations in instability platforms, check out the OPTP PRO-PODS™.
Uneven surface balance tools
As mentioned, one major consideration in today’s balance training program development is the functionality of exercises. That is, how does, “balance exercise x” help prepare the patient or client for doing, “activity x” in their day-to-day life?
Because most people spend a fair amount of time standing, walking, hiking, jogging, or running on surfaces that are not unstable, innovators recently began creating products that offer uneven surfaces. Balance tools with an uneven surface offer variability that is more similar to what people might encounter in their daily lives including hills, uneven grass or playing fields, rocky walkways, old sidewalks, and hiking trails.
These surfaces have fixed and unfixed obstacles that people must navigate on, over and across safely. Moving on and across an uneven surface offers the same benefits that unstable surfaces offer, with the added benefit of increased functionality. To train on any uneven surface, people would normally have to venture outside to the nearest park, trail, hill, field, or mountain; until now.
CobbleFoam: A highly effective approach to improving balance
OPTP recently released an innovative new balance training product called CobbleFoam. Each CobbleFoam board is 16” x 16” and features foam blocks of varying heights that create uneven terrain to stand on or traverse across. The CobbleFoam board/s simulate the uneven surfaces we encounter in everyday life and can be used safely and comfortably in the clinic, studio, gym or home.
Conducting any balance exercise on an uneven surface like CobbleFoam immediately increases the benefits of the movement. Due to the variability of the uneven surface, the brain and muscles will be engaged at a deeper level to keep the body upright and balanced. In addition, the deep intrinsic stability system of the foot-ankle-knee complex will be activated to a much greater degree, building strength and joint integrity.
To make balance exercises even more functional and life-like, combining an uneven surface like the CobbleFoam board/s with other fitness tools like weights, steps, balance pads and hurdles to develop an “obstacle course” is a highly effective approach to developing and improving functional balance.
The key to the most profound overall benefits
The use of both unstable and uneven balance training products offers incredibly beneficial outcomes for patients and clients. When combined with functional movement that is most similar to activities of daily life, patients and clients will realize the most profound overall benefits.
To explore all of OPTP’s 40+ balance training products, visit optp.com.